Overview
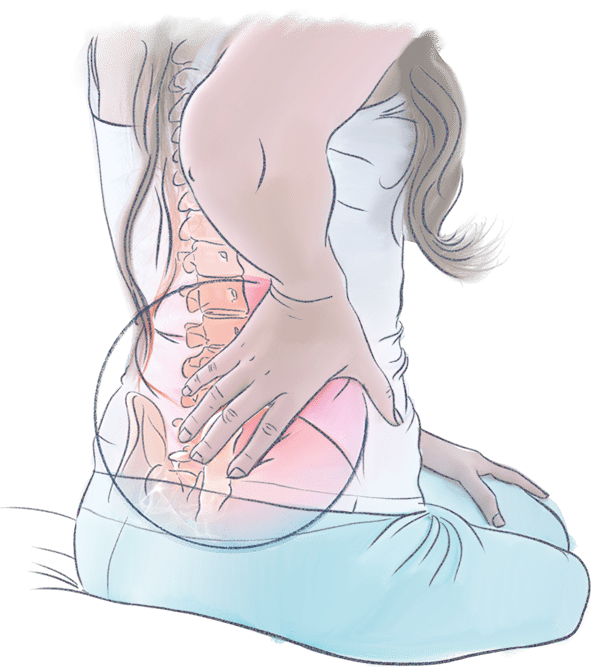
Lower back pain is very common, but is nonetheless a serious health concern for many; one which can have a significant impact on your quality of life.
It can range from a persistent dull ache to a sudden, sharp or shooting pain. It can come on suddenly – perhaps after an accident or physical trauma – or it can develop slowly due to age-related degeneration. In some cases, parallel medical conditions can intensify symptoms.
Around 80% of all people will suffer with some form of lower back pain at some point during their lives, involving pathologies – problems – that impact some combination of their muscles, nerves, and bones.
Bone and joint conditions that lead to lower back pain can be classified in several ways:
- Congenital, if present in some form since birth
- Degenerative, if resulting from wear and tear
- Traumatic, if caused by injury
Symptoms are often caused by spinal instability, or by disc, bone or ligaments pressing onto nervous tissue.
Treatments vary depending on the cause and symptoms, but there are steps you can take to improve your health, reduce discomfort, and lower your chance of developing chronic or long-lasting back pain.
Who suffers from back pain?
The short answer is that anyone and everyone can develop back pain, but there are several factors that may affect your personal level of risk.
Types of back pain
Doctors tend to describe instances of back pain in one of three ways:
- Acute pain comes on suddenly and passes relatively quickly, lasting from a few moments or hours, to at most a few days
- Subacute pain can follow a similar initial pattern to ‘acute’ pain, but lasting for between 4 and 12 weeks. This kind of pain can also develop more slowly over that period.
- Chronic pain may present quickly or slowly, but tends to be associated with pain lasting longer than 12 weeks.
Symptoms of back pain
Back pain can be localised to a specific spot, generalized, spreading all over the back, or radial, following nerve pathways away from the back to other areas of the body, including the buttocks, legs, or abdomen. The intensity of back pain varies from person to person.
Depending on the type, cause, and location of your back pain, you may experience:
- Increased pain when moving or performing physical tasks
- Worsening pain when resting, sitting, or standing still for extended periods
- Back pain that comes and goes in waves
- Pain that lessens with normal daily tasks as muscles stretch and tightness reduces
- Pain that radiates away from your back into the buttocks, leg, or hips
- Numbness and tingling in your lower back, torso, or legs.
Conditions
Back pain can come on suddenly – perhaps after an accident or physical trauma – or it can develop slowly because of age-related degeneration to vital structures in the spine. In some cases, inflammatory conditions or other parallel medical conditions can intensify symptoms.
Structural Problems
Back pain can happen when problems develop in the spine’s anatomical structure – the bones, discs, muscles, ligaments, or tendons in the back.
Some instances of back pain will resolve with rest – these may include relatively minor strains or sprains, which usually impact the muscles, ligaments or tendons around the spinal column after some form of sudden or strenuous activity.
Other conditions are, however, more serious, and may require surgical intervention to affect long-term relief of symptoms. These may include one or a combination of the following:

Degenerative disc disease occurs when the supportive, intervertebral discs break down over time, reducing their ability to comfortably support everyday movement, leading to nerve compression and, sometimes, releasing proteins that irritate surrounding nerves.

Spinal stenosis refers to a narrowing of the spinal column that puts pressure on the spinal cord and nerves. This can happen as a result of arthritis, degenerative disc disease, spondylolisthesis, or similar conditions associated with spinal instability

Herniated or ruptured discs: A loss of integrity in the discs compress and irritate nearby nerves. This most commonly occurs in the lower, ‘lumbar’ region of the spine.

Vertebral compression fractures happen when the body of a vertebra in the spine collapses, often leading to severe pain, deformity and, occasionally, loss of height. These fractures most commonly occur in the middle, thoracic section of the spine, and often result from osteoporotic bone weaking.

Spondylolisthesis is the name given to a vertebra slipping out of place, compressing surrounding nerves. This can happen at any point along the spine, but happens most commonly in the lumbar region.
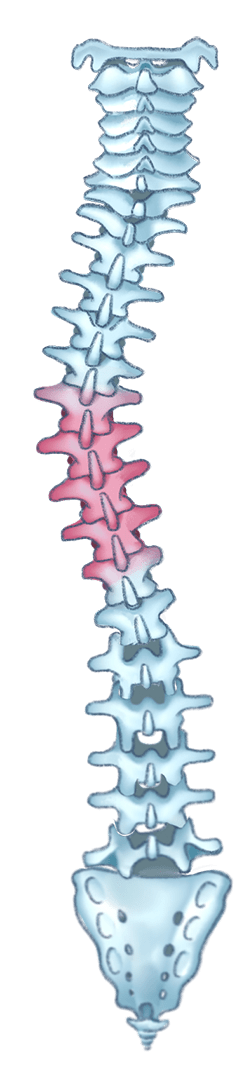
Deformity, whether idiopathic or degenerative, when the spine is shaped in such a way to compromise movement, cause visible physical deformity, or discomfort.
What are my Treatment Options?
The best course of action in treating your specific spinal health concern will depend on many factors, including:
- Your condition
- Your age
- Your medical history
- Whether you currently have any other health concerns
Your physician will be able to determine the treatment best suited to you and your individual situation.
Back pain can often be treated with a combination of ‘conservative’, non-surgical treatments, such as manual therapy, exercise, medication, and lifestyle changes.
If symptoms do not improve after conservative treatment, or if your circumstances are such that they are not suitable, your doctor may recommend surgical treatment to improve your spine’s stability.
By supporting any weakened parts of the spine, and removing sources of pressure on a patient’s nervous system, surgical intervention can provide effective relief from fracture related discomfort, helping you back to better health and a higher quality of life.


